Connect With Us
Blog
Items filtered by date: April 2022
Two Types of Plantar Warts

It can be easy to notice a plantar wart, which is a small, hardened area on the bottom of the foot. They may have tiny black dots in the center and grow into the foot as a result of the pressure that is exerted by standing and walking. The medical term for this ailment is verruca plantaris, and it is caused by the human papillomavirus (HPV). It is considered to be contagious, and enters the body through small cracks in the skin of the feet. Research has shown there are two types of plantar warts. A single plantar wart is classified as a solitary plantar wart, though smaller warts may form from it. Mosaic plantar warts are found in clusters and may require more extensive treatment methods. Patients who have compromised immune systems may be susceptible to developing these types of warts, in addition to children and older people. Prevention techniques can include wearing appropriate footwear while in public shower rooms, locker rooms, or swimming pools. If you think you have plantar warts, it is suggested that you confer with a podiatrist who can provide you with correct treatment options.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Nassau Foot & Ankle. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Oceanside, Franklin Square, and East Norwich, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding an Achilles Tendon Rupture
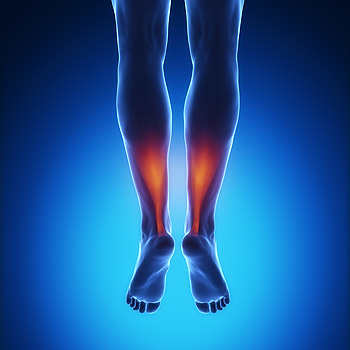 An Achilles tendon rupture is an injury that happens when there is sudden and overwhelming pressure put on the Achilles tendon – the band of fibrous tissue that links the muscles of the calf to the heel. There will usually be a popping noise and intense pain with this injury and the area may burn and become swollen and stiff. You will have trouble standing and pushing off from that leg. Rest, cold compresses, physical therapy, and attention to a proper diet can all help, but this condition is slow to heal. A podiatrist can perform what is known as the Thompson Test to determine if you have ruptured your Achilles tendon. This test consists of a simple manipulation of the back of the calf, specifically, your soleus complex muscle group. If the area does not tense up and bend (a natural reflex of the manipulation), you may have ruptured this major tendon or there has been a detachment of the tendon from the muscle or bone. A consultation with a podiatrist is suggested if you suspect you have injured or ruptured your Achilles tendon for a proper treatment plan.
An Achilles tendon rupture is an injury that happens when there is sudden and overwhelming pressure put on the Achilles tendon – the band of fibrous tissue that links the muscles of the calf to the heel. There will usually be a popping noise and intense pain with this injury and the area may burn and become swollen and stiff. You will have trouble standing and pushing off from that leg. Rest, cold compresses, physical therapy, and attention to a proper diet can all help, but this condition is slow to heal. A podiatrist can perform what is known as the Thompson Test to determine if you have ruptured your Achilles tendon. This test consists of a simple manipulation of the back of the calf, specifically, your soleus complex muscle group. If the area does not tense up and bend (a natural reflex of the manipulation), you may have ruptured this major tendon or there has been a detachment of the tendon from the muscle or bone. A consultation with a podiatrist is suggested if you suspect you have injured or ruptured your Achilles tendon for a proper treatment plan.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Nassau Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Oceanside, Franklin Square, and East Norwich, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Who Is Prone to Sever’s Disease?
 The medical term for the growth area where the plantar fascia and the Achilles tendon connect to the heel is known as the calcaneal apophysis. It starts to develop in children approximately 7 or 8 years old, and permanently fuses to the heel bone in young teenagers. Children in this age group who frequently participate in sports activities may experience a condition that is known as Sever’s disease. Common symptoms of this ailment can include intense heel pain, which can become worse when wearing shoes that have limited cushioning or arch support. Sever's disease is an irritation of the heel, which occasionally causes swelling and bruising. Successful treatment options include temporarily stopping the activity that caused the injury and resting the affected foot as often as possible. Some patients perform specific stretches that may help to increase flexibility. If you have Sever’s disease, it is suggested that you are under the care of a podiatrist who can guide you toward correct treatment options.
The medical term for the growth area where the plantar fascia and the Achilles tendon connect to the heel is known as the calcaneal apophysis. It starts to develop in children approximately 7 or 8 years old, and permanently fuses to the heel bone in young teenagers. Children in this age group who frequently participate in sports activities may experience a condition that is known as Sever’s disease. Common symptoms of this ailment can include intense heel pain, which can become worse when wearing shoes that have limited cushioning or arch support. Sever's disease is an irritation of the heel, which occasionally causes swelling and bruising. Successful treatment options include temporarily stopping the activity that caused the injury and resting the affected foot as often as possible. Some patients perform specific stretches that may help to increase flexibility. If you have Sever’s disease, it is suggested that you are under the care of a podiatrist who can guide you toward correct treatment options.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see one of our podiatrists from Nassau Foot & Ankle. Our doctors can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Oceanside, Franklin Square, and East Norwich, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Are Bunions Affecting Your Everyday Life?
What Might Be Causing Your Heel Pain
Heel pain—and pain at the back of the feet—in older adults can typically be caused by plantar fasciitis, Achilles tendon injuries, or various types of bursitis. Plantar fasciitis causes pain and stiffness at the bottom of heel, when the plantar fascia tissue that attaches there becomes damaged/torn and inflamed. It can typically be treated by night splinting to keep the plantar fascia in a neutral position, custom orthotics, corticosteroid injections, physical therapy, shockwave therapy, and more. Bursitis is an inflammation of one of the bursas in the feet. Bursas are sacs filled with fluid that provide cushioning between bones and tendons and help reduce friction between bones. Bursitis in the feet can occur either where the plantar fascia or the Achilles tendon attaches to the heel bone, or in response to pressure from shoes at the back of the foot. These conditions can often be treated with footwear modifications, heel pads, gel wraps, orthotics and padding, corticosteroid injections, physical therapy, night splints, non-steroidal anti-inflammatory drugs, cold or warm compresses and more. If you have any type of pain in your heel, call a podiatrist. They are experts at diagnosing and treating all forms of heel pain.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Nassau Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Oceanside, Franklin Square, and East Norwich, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Do You Have Poor Blood Circulation in Your Feet?
 Seniors are particularly susceptible to poor blood circulation that can often affect the feet. Symptoms to look for in checking your feet for poor circulation are numbness, tenderness, cramping, swelling, coldness, and discoloration (paleness, white patches on skin and toenails), particularly after physical activity or prolonged standing. It should be considered a critical situation if your feet turn blue as this usually means they are not receiving enough oxygen due to poor circulation. If you have wounds on your feet that are slow to heal, this can also be a sign that blood circulation to your feet is problematic. As one ages, and foot problems become more common, it is a good idea to visit a podiatrist regularly to have your feet examined and tended to. It is particularly important to seek treatment if you suspect poor blood circulation in the feet because, if left untreated, serious problems such as varicose veins and amputation can result.
Seniors are particularly susceptible to poor blood circulation that can often affect the feet. Symptoms to look for in checking your feet for poor circulation are numbness, tenderness, cramping, swelling, coldness, and discoloration (paleness, white patches on skin and toenails), particularly after physical activity or prolonged standing. It should be considered a critical situation if your feet turn blue as this usually means they are not receiving enough oxygen due to poor circulation. If you have wounds on your feet that are slow to heal, this can also be a sign that blood circulation to your feet is problematic. As one ages, and foot problems become more common, it is a good idea to visit a podiatrist regularly to have your feet examined and tended to. It is particularly important to seek treatment if you suspect poor blood circulation in the feet because, if left untreated, serious problems such as varicose veins and amputation can result.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact one of our podiatrists of Nassau Foot & Ankle. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our offices located in Oceanside, Franklin Square, and East Norwich, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021


